Explore Revolutionary Discoveries in Nitric Oxide Synthesis Techniques
Unlocking New Enzymatic Pathways to Enhance Nitric Oxide Production
Recent breakthroughs in nitric oxide research updates have unveiled innovative enzymatic pathways that are critical for the effective synthesis of nitric oxide. These discoveries have significant implications not only for fundamental scientific inquiry but also for practical applications in clinical settings. Researchers have identified a diverse array of enzymes beyond the conventional nitric oxide synthases (NOS), unveiling a sophisticated biochemical network that regulates nitric oxide production across various tissues. This expanded understanding suggests that nitric oxide synthesis is not limited to endothelial cells lining blood vessels but can also occur in a multitude of other cells, including neurons and immune cells. Such revelations are essential for appreciating the broader biological significance of nitric oxide in health and disease.
The implications of these findings are extensive, especially regarding our understanding of nitric oxide’s pivotal role in health and disease pathology. For example, in the realm of cardiovascular health, the newly discovered pathways could pave the way for the development of targeted therapies designed to elevate nitric oxide levels in conditions such as hypertension and heart disease. Moreover, this enriched knowledge about nitric oxide synthesis pathways equips scientists with essential tools to explore its involvement in cellular signaling, inflammation, and even the advancement of cancer. Ongoing research continues to deepen our comprehension of nitric oxide, underscoring the dynamic mechanisms that regulate its synthesis and the exciting potential for innovative treatment modalities.
Transforming Nitric Oxide Synthesis Approaches for Greater Efficiency
The advancement of nitric oxide synthesis techniques has experienced extraordinary growth, markedly improving production efficiency and opening doors to revolutionary medical and industrial applications. Recent investigations have shown that refining chemical synthesis methodologies can result in the generation of nitric oxide in a more regulated and sustainable manner. These enhancements are not merely technical feats; they carry profound implications for therapeutic interventions. For instance, the enhanced capacity to produce nitric oxide efficiently means it can be utilized in clinical environments for a broader array of conditions, potentially transforming existing treatment approaches into more effective strategies.
Additionally, these advanced synthesis techniques are crucial in minimizing the environmental impact typically associated with traditional chemical production methods. By optimizing these processes, researchers can significantly reduce waste and conserve energy, aligning with global sustainability efforts. The adoption of these refined synthesis techniques is vital not only for research initiatives but also for the commercial viability of nitric oxide products, which encompass pharmaceuticals, dietary supplements, and agricultural applications. The ability to produce nitric oxide more sustainably could revolutionize diverse industries, reinforcing its importance as an essential molecule in both health and environmental contexts.
Innovative Catalysts Leading the Future of Nitric Oxide Synthesis
The pursuit of more effective catalysts for nitric oxide synthesis has sparked exciting innovations within the scientific community. Researchers are actively investigating novel catalysts that can significantly enhance the efficiency and selectivity of nitric oxide production. Many of these groundbreaking catalysts are derived from metal-organic frameworks and other advanced materials, which facilitate the essential conversion processes needed for generating nitric oxide. The ramifications of these advancements stretch across various fields, particularly in medicine, where improved delivery methods for nitric oxide could yield enhanced therapeutic outcomes for patients.
One significant advantage of utilizing these innovative catalysts is their capacity to reduce the activation energy necessary for nitric oxide synthesis, allowing reactions to take place under milder conditions. This shift could translate into more cost-effective and accessible production methods, particularly benefiting developing regions where resources may be limited. Furthermore, the choice of catalysts has a considerable impact on potential side reactions during synthesis, making selectivity a crucial factor in developing safe and effective nitric oxide therapies. As research progresses, these advanced catalysts could play a pivotal role in drug development, especially for conditions where nitric oxide is known to provide beneficial effects, such as in cardiovascular and pulmonary diseases.
Understanding Nitric Oxide’s Vital Role in Cardiovascular Health
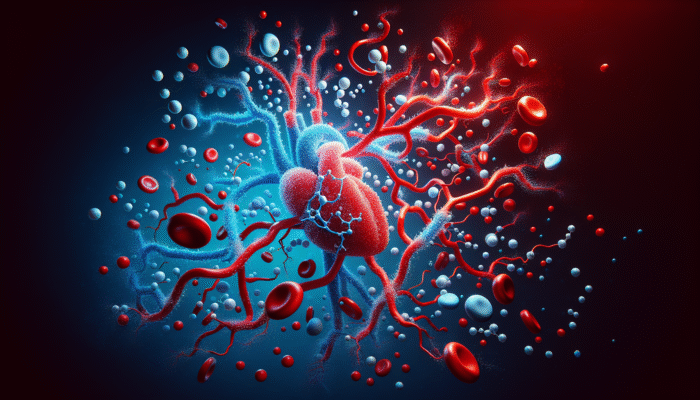
Vasodilation Mechanisms: How Nitric Oxide Regulates Blood Flow
Vasodilation, the physiological process responsible for the widening of blood vessels, is significantly influenced by nitric oxide. This essential molecule functions as a signaling agent that facilitates relaxation in the smooth muscle of blood vessels, thereby enhancing blood flow and reducing blood pressure. Recent studies have enriched our understanding of the intricate mechanisms involved in vasodilation, uncovering complex signaling pathways that highlight nitric oxide’s interactions with various receptors and cellular components. The discovery of additional pathways emphasizes the fundamental role of nitric oxide in sustaining vascular health, showcasing its significance as a natural regulator of cardiovascular function.
The ramifications of these findings are far-reaching, as they open potential avenues for therapeutic intervention in conditions characterized by impaired vasodilation, such as hypertension and atherosclerosis. By enhancing nitric oxide production or mimicking its effects, researchers are exploring innovative treatment strategies designed to restore normal vascular function in patients afflicted with cardiovascular diseases. Furthermore, nitric oxide’s influence extends beyond mere vasodilation; it is also integral to processes such as platelet aggregation and leukocyte adhesion, both of which are critical for maintaining vascular integrity and functionality, thus reinforcing the importance of this molecule in cardiovascular health.
Exploring Nitric Oxide’s Impact on Heart Function and Efficiency
The influence of nitric oxide on heart function represents a burgeoning area of research, emphasizing its critical role in regulating blood flow, along with the contractility and relaxation of cardiac muscle. Studies have demonstrated that nitric oxide modulates the heart’s response to stress, ensuring it can adapt to varying physiological demands. The molecule’s ability to promote smooth muscle relaxation and reduce myocardial oxygen consumption underscores its significance in maintaining cardiac efficiency, particularly during physical exertion and increased activity levels.
Recent discoveries suggest that nitric oxide may also confer protective effects in instances of heart failure by enhancing relaxation and decreasing the overall workload on the heart. This has substantial implications for heart disease treatment, as therapies aimed at increasing nitric oxide bioavailability could provide symptomatic relief and improve overall heart function for affected patients. By elucidating the pathways through which nitric oxide influences cardiac contractility, researchers are laying the groundwork for innovative treatments that capitalize on its protective and regulatory effects, ultimately enhancing patient care and outcomes.
Harnessing the Therapeutic Potential of Nitric Oxide in Cardiovascular Disease Management
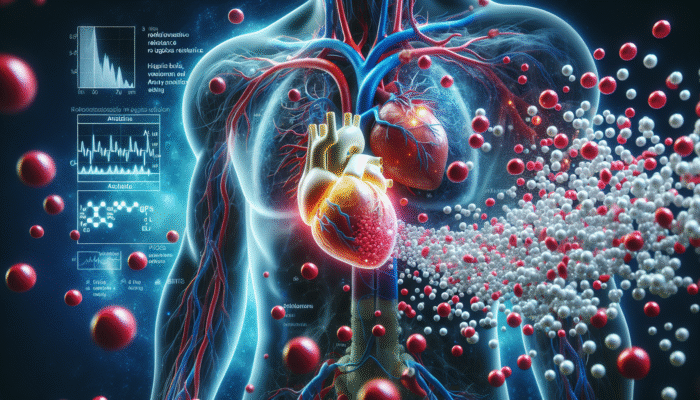
The therapeutic potential of nitric oxide in combating cardiovascular diseases has garnered significant attention in recent years, fueled by accumulating evidence supporting its efficacy. Clinical studies have illustrated that nitric oxide donors can substantially enhance outcomes in conditions such as angina, heart failure, and pulmonary hypertension. These therapies operate by increasing blood flow and reducing vascular resistance, ultimately providing symptom relief and enhancing the quality of life for patients.
In addition to immediate therapeutic applications, ongoing research is exploring the long-term benefits of sustained nitric oxide delivery. This approach could revolutionize the management of chronic cardiovascular conditions by providing a continuous supply of this vital molecule to support endothelial health and prevent disease progression. Moreover, investigating nitric oxide’s role in preventing atherosclerosis and other cardiovascular complications underscores its potential as a preventive strategy. As researchers continue to decode the mechanisms through which nitric oxide exerts its effects, the prospect of developing cutting-edge therapies that harness its benefits appears increasingly promising, offering hope for better patient outcomes.
Enhancing Endothelial Function with Nitric Oxide
The endothelium, the delicate cellular layer lining blood vessels, is critical for cardiovascular health, and nitric oxide emerges as a key regulator of endothelial function. This molecule not only promotes vasodilation but also provides protective effects against endothelial dysfunction, which serves as a precursor to various cardiovascular diseases. Recent studies have illuminated the intricate interactions between nitric oxide and endothelial cells, showcasing its role in modulating inflammation, inhibiting platelet aggregation, and regulating vascular permeability, all of which are vital for maintaining vascular homeostasis.
A deeper understanding of nitric oxide’s influence on endothelial function uncovers opportunities for therapeutic intervention in conditions marked by endothelial dysfunction, such as diabetes and hypertension. Strategies aimed at enhancing nitric oxide bioavailability could mitigate the adverse effects associated with these conditions, ultimately promoting vascular health and reducing the risk of cardiovascular events. Furthermore, the complex relationship between nitric oxide and other signaling molecules, such as reactive oxygen species, adds layers of complexity to our understanding of endothelial biology, emphasizing the importance of continued research in this critical area.
Examining Nitric Oxide’s Role in Neurological Disorders
The Neuroprotective Advantages of Nitric Oxide in Neurological Health
The neuroprotective properties of nitric oxide are garnering increased attention in ongoing research, particularly regarding its potential to shield neurons from damage in various neurological disorders. Nitric oxide plays a crucial role in signaling pathways that support neuronal survival and facilitate repair mechanisms in response to injury. Recent studies have underscored its protective effects against excitotoxicity, oxidative stress, and inflammation, all of which are commonly associated with neurodegenerative diseases, thereby highlighting its importance in maintaining neurological health.
For instance, research has demonstrated that nitric oxide can regulate the activity of neurotrophic factors, which are essential for promoting neuronal growth and differentiation. This suggests that enhancing nitric oxide levels or mimicking its effects could yield therapeutic advantages in conditions such as Alzheimer’s and Parkinson’s diseases. Furthermore, neuroprotective strategies centered around nitric oxide may bolster recovery from neural injuries, providing renewed hope for rehabilitation in patients who have experienced strokes or traumatic brain injuries, thus expanding its therapeutic potential.
Diving Deeper into Nitric Oxide’s Role in Neuroinflammation
Neuroinflammation is a defining characteristic of numerous neurological conditions, and nitric oxide plays a pivotal role in its regulation. While nitric oxide can provide protective effects, it may also promote inflammatory responses when produced in excessive amounts. Recent studies have clarified this dual role, revealing how nitric oxide signaling can influence the activity of glial cells and immune responses within the brain. Understanding nitric oxide’s role in neuroinflammation is vital for developing targeted therapies that can mitigate its detrimental effects while preserving its beneficial functions, thus enhancing treatment strategies for neurodegenerative conditions.
Investigating nitric oxide’s involvement in neuroinflammation has significant implications for managing disorders such as multiple sclerosis, Alzheimer’s disease, and traumatic brain injury. By targeting specific signaling pathways influenced by nitric oxide, researchers aim to create strategies that can effectively modulate inflammation in the nervous system, thereby enhancing neuronal survival and functionality. These insights not only advance our understanding of neuroinflammatory processes but also inform the development of innovative treatment modalities aimed at improving outcomes for individuals affected by neurological disorders, paving the way for new therapeutic avenues.
Exploring Innovative Treatments for Neurological Conditions Utilizing Nitric Oxide
The exploration of nitric oxide-based treatments for neurological conditions is gaining momentum, driven by promising results from clinical trials. Researchers are investigating various delivery methods for nitric oxide, including inhalation therapies and transdermal patches, designed to navigate the challenges posed by its rapid degradation within the body. These innovative approaches have the potential to amplify the therapeutic efficacy of nitric oxide, providing new hope for patients suffering from conditions such as migraines, chronic pain, and neurodegenerative diseases, thus broadening its clinical application.
Moreover, the potential for nitric oxide to serve as a biomarker for neurological conditions is currently under exploration. Studies suggest that altered nitric oxide levels may correlate with disease progression in certain disorders, offering a valuable tool for monitoring treatment responses and disease status. As the field of nitric oxide research progresses, clinicians and researchers are eager to translate these findings into practical applications that can enhance the quality of life for those affected by neurological conditions, reinforcing the molecule’s significance in modern medicine.
Impact of Nitric Oxide on Neurodegenerative Diseases
The role of nitric oxide in neurodegenerative diseases, particularly concerning Alzheimer’s and Parkinson’s, is an emerging area of intense investigation. Recent studies indicate that dysregulation of nitric oxide signaling may contribute to the pathogenesis of these disorders, implicating it in critical processes such as amyloid plaque formation and mitochondrial dysfunction. Understanding these mechanisms is essential for developing targeted therapies that can leverage the protective effects of nitric oxide while mitigating its harmful consequences, thus enhancing treatment options for patients.
Innovative strategies are being explored to enhance nitric oxide delivery to the brain, which could hold promise for slowing the progression of neurodegenerative diseases. For instance, certain pharmacological agents are being developed to specifically boost nitric oxide synthesis within neural tissues, allowing for a targeted therapeutic effect. The potential to harness nitric oxide’s neuroprotective properties could revolutionize treatment options available for patients facing these debilitating conditions, providing hope for improved management and a better quality of life.
Deciphering Nitric Oxide Signaling Pathways in Neurology
A comprehensive understanding of nitric oxide signaling pathways is critical for developing targeted therapies aimed at neurological disorders. These pathways influence various aspects of neuronal function, including neurotransmitter release, synaptic plasticity, and cell survival. Recent research has identified key molecules involved in nitric oxide signaling, such as soluble guanylate cyclase and cyclic GMP, which serve as essential mediators of its effects, thus providing insight into its multifaceted role in the nervous system.
By elucidating these signaling pathways, researchers can identify potential therapeutic targets for modulating nitric oxide’s effects in neurological contexts. For instance, enhancing the activity of nitric oxide signaling pathways could confer neuroprotective benefits, while inhibiting excessive signaling might mitigate inflammatory responses linked to neurodegenerative diseases. As our understanding of nitric oxide signaling continues to deepen, the potential for developing innovative therapies that leverage this knowledge becomes increasingly feasible, paving the way for novel interventions in neurology.
The Essential Role of Nitric Oxide in Respiratory Health
Understanding Nitric Oxide’s Mechanisms in Lung Function and Health
Nitric oxide plays an indispensable role in maintaining respiratory health, particularly through its mechanisms in lung function. This molecule is produced by the epithelial cells lining the airways and serves as a potent vasodilator, enhancing blood flow in the lungs and facilitating efficient gas exchange. Recent studies have illuminated the complex mechanisms by which nitric oxide regulates airway tone, inflammation, and pulmonary vascular resistance, emphasizing its multifaceted role in respiratory physiology and overall lung health.
A significant aspect of nitric oxide’s function in the lungs is its involvement in modulating airway hyperreactivity, a characteristic feature of conditions such as asthma and other respiratory disorders. By promoting relaxation of airway smooth muscle, nitric oxide contributes to bronchodilation, alleviating symptoms and enhancing airflow. Understanding these mechanisms not only enriches our comprehension of respiratory health but also informs the development of targeted therapies aimed at harnessing nitric oxide’s benefits for individuals suffering from chronic respiratory conditions, thereby improving their quality of life.
Exploring Therapeutic Applications of Nitric Oxide in Respiratory Conditions
The therapeutic applications of nitric oxide in addressing respiratory conditions are gaining significant attention, with clinical studies demonstrating its efficacy in various settings. One of the most notable uses of nitric oxide therapy is in the treatment of pulmonary hypertension, where inhaled nitric oxide has been shown to markedly improve oxygenation and reduce pulmonary vascular resistance. This approach has proven particularly beneficial for patients with conditions such as congenital heart defects and acute respiratory distress syndrome, showcasing nitric oxide’s potential as a life-saving intervention.
Beyond pulmonary hypertension, researchers are investigating the potential of nitric oxide in treating asthma, chronic obstructive pulmonary disease (COPD), and other respiratory disorders. By leveraging the bronchodilatory effects of nitric oxide, clinicians may provide patients with a novel therapeutic option that complements existing treatments. The development of portable delivery systems for inhaled nitric oxide also holds promise, enabling wider access to this therapy for individuals in diverse clinical settings worldwide, thus expanding its impact on respiratory health.
Investigating the Impact of Nitric Oxide on Pulmonary Hypertension
Recent research has emphasized the significant impact of nitric oxide in managing pulmonary hypertension, a condition characterized by elevated blood pressure in the pulmonary arteries. Nitric oxide therapy has emerged as a cornerstone in treating this condition, demonstrating remarkable efficacy in promoting vasodilation and improving exercise capacity. Clinicians have observed substantial improvements in symptoms and quality of life for patients receiving inhaled nitric oxide, reinforcing its role as a vital therapeutic agent in respiratory health and patient management.
The mechanisms through which nitric oxide exerts its effects in pulmonary hypertension are multifaceted. By enhancing endothelial function and reducing vascular resistance, nitric oxide not only alleviates symptoms but also addresses the underlying pathophysiology of the disease. Ongoing research focuses on optimizing nitric oxide delivery methods and exploring combination therapies that may further enhance its effectiveness. As our understanding of pulmonary hypertension evolves, the therapeutic potential of nitric oxide continues to be a focal point in respiratory health research, offering new hope for patients.
Revealing the Antimicrobial Properties of Nitric Oxide
Understanding Mechanisms of Action Against Pathogens
The antimicrobial properties of nitric oxide have garnered increasing attention, revealing its potential as a powerful agent against a diverse range of pathogens. Research has demonstrated that nitric oxide can disrupt the integrity of microbial membranes, leading to cell death in bacteria, viruses, and fungi. This mechanism of action positions nitric oxide as a valuable asset in the fight against infectious diseases, with potential applications spanning both clinical and environmental contexts, thus highlighting its versatility as an antimicrobial agent.
One area of investigation focuses on how nitric oxide interacts with the immune system to amplify its antimicrobial effects. By modulating the activity of immune cells, such as macrophages and neutrophils, nitric oxide orchestrates a coordinated response against infections. Understanding these interactions can pave the way for developing nitric oxide-based therapies that enhance the body’s natural defenses against pathogens, offering innovative strategies for infection control in an era marked by rising antibiotic resistance, thus addressing a critical public health challenge.
Applications of Nitric Oxide in Infection Control Strategies
The application of nitric oxide in infection control strategies is an exciting frontier in medical research. Clinical studies have explored its use in wound care, where nitric oxide’s antimicrobial properties can enhance healing and prevent infection in chronic wounds. By delivering nitric oxide locally to affected areas, clinicians can leverage its potent effects to combat antibiotic-resistant pathogens and promote tissue regeneration, thereby improving patient outcomes and accelerating recovery.
Additionally, researchers are investigating the potential for utilizing nitric oxide in sanitization and disinfection processes. Given its broad-spectrum antimicrobial activity, nitric oxide could serve as an effective alternative to traditional disinfectants in various settings, including healthcare facilities and public spaces. The ongoing research into nitric oxide’s applications in infection control underscores its versatility and the promise it holds for enhancing public health outcomes globally, especially in combating the spread of infectious diseases.
Future Directions in Antimicrobial Research Involving Nitric Oxide
As our understanding of nitric oxide’s antimicrobial properties expands, future research directions are being outlined to explore its full potential. Scientists are investigating novel delivery methods, such as nanoparticle-based systems, which can enhance the stability and bioavailability of nitric oxide. These innovative strategies could pave the way for more effective therapies that incorporate nitric oxide into existing treatment regimens for infections, thereby improving patient care and outcomes.
Furthermore, ongoing studies are examining the synergistic effects of combining nitric oxide with other antimicrobial agents. This strategy aims to boost treatment efficacy and address the growing concern of antimicrobial resistance. By unlocking the full potential of nitric oxide in this context, researchers aspire to develop new therapeutic options that significantly improve patient outcomes and tackle the challenges posed by resistant pathogens, thus enhancing the overall effectiveness of infection management strategies.
Exploring Synergistic Effects with Other Antimicrobials
The exploration of synergistic effects between nitric oxide and other antimicrobial agents represents a promising area of study, with potential implications for enhancing treatment outcomes. Research has revealed that combining nitric oxide with antibiotics can lead to increased efficacy against resistant strains of bacteria, potentially reversing antibiotic resistance mechanisms. This synergy may allow for reduced doses of antibiotics, minimizing the risk of side effects while maintaining therapeutic effectiveness, thus providing a more sustainable approach to infection treatment.
Incorporating nitric oxide into existing treatment protocols could also enhance patient outcomes across various infectious diseases, ranging from bacterial infections to viral outbreaks. By understanding the mechanisms underlying these synergistic interactions, researchers can develop targeted combination therapies that harness the unique properties of both nitric oxide and conventional antimicrobial agents. This approach is a vital step toward addressing the pressing global challenge of antimicrobial resistance, offering new hope for effective infection control.
Clinical Trials and Case Studies on Nitric Oxide’s Antimicrobial Applications
Ongoing clinical trials and case studies are crucial for evaluating the effectiveness of nitric oxide in real-world antimicrobial applications. Researchers are actively monitoring the outcomes of nitric oxide therapies across diverse patient populations, assessing their safety and efficacy in treating various infections. These studies provide valuable insights into the clinical utility of nitric oxide and inform the development of standardized treatment protocols, thereby enhancing its applicability in clinical settings.
Preliminary results from these trials have shown promise, indicating that nitric oxide can reduce infection rates and promote faster healing in patients with chronic wounds and respiratory infections. The growing body of evidence supports the integration of nitric oxide into infection control strategies, reinforcing its potential as a key player in combating infections. As clinical research progresses, the future of nitric oxide in antimicrobial therapies appears bright, offering hope for innovative solutions to tackle infectious diseases effectively.
Nitric Oxide’s Role in Cancer Research and Treatment
Understanding Nitric Oxide’s Dual Role in Tumor Growth and Regulation
The role of nitric oxide in tumor growth represents a complex and multifaceted area of research, shedding light on its dual nature within cancer biology. While nitric oxide is known to facilitate angiogenesis—the process through which tumors develop their blood supply—it also exerts anti-tumor effects by inducing apoptosis in cancer cells. Recent studies have investigated the intricate mechanisms by which nitric oxide influences tumor development and progression, revealing its potential as both a facilitator and a regulator of cancer biology, thus presenting opportunities for targeted therapeutic interventions.
Understanding the delicate balance between nitric oxide’s pro-tumor and anti-tumor effects is essential for developing targeted therapies in cancer treatment. Researchers are exploring how modulating nitric oxide levels can influence tumor metabolism, growth, and response to chemotherapy. By harnessing its effects, there is potential to formulate innovative strategies that leverage nitric oxide to inhibit tumor growth while simultaneously enhancing the efficacy of existing therapies, thereby improving treatment outcomes for cancer patients.
Investigating Nitric Oxide’s Potential in Cancer Therapy
The potential of nitric oxide as a cancer therapy is receiving increasing attention, with ongoing research exploring its applications across various cancer types. Preclinical studies have demonstrated that nitric oxide donors can selectively induce cancer cell death while sparing healthy cells, positioning nitric oxide as a promising candidate for targeted cancer therapies. This selectivity is particularly appealing, as it may help mitigate the side effects commonly associated with conventional cancer treatments, thus enhancing patient quality of life.
Innovative strategies are being explored to facilitate nitric oxide delivery directly to tumor sites, maximizing its therapeutic effects while minimizing systemic exposure. By tailoring nitric oxide delivery systems, researchers aim to enhance its efficacy as an adjunct therapy for patients undergoing chemotherapy or radiation treatment. As our understanding of nitric oxide’s role in cancer biology continues to evolve, the potential for developing nitric oxide-based therapies appears increasingly promising, offering new hope for patients facing a cancer diagnosis and improving their treatment options.
Understanding Nitric Oxide’s Impact on Metastasis
The impact of nitric oxide on metastasis, which involves the spread of cancer cells to distant sites, is an area of growing investigation. Recent studies suggest that nitric oxide may influence various processes integral to metastasis, including cell invasion, migration, and the establishment of secondary tumors. Understanding these mechanisms is critical for developing therapeutic strategies aimed at preventing or reducing metastatic spread, a leading cause of cancer-related mortality, thus highlighting the importance of nitric oxide in cancer research.
Researchers are actively exploring how modulating nitric oxide levels can alter the metastatic potential of cancer cells, thereby offering new avenues for intervention. By targeting nitric oxide signaling pathways, it may be feasible to inhibit the processes that facilitate metastasis, ultimately improving patient outcomes. As the field of cancer research continues to unravel the complexities surrounding nitric oxide’s role in tumor biology, the potential for innovative therapies targeting metastasis becomes increasingly plausible, paving the way for advanced cancer treatments.
Examining Nitric Oxide’s Effects on the Tumor Microenvironment
The tumor microenvironment is a crucial factor influencing cancer progression, and nitric oxide plays a significant role in shaping this environment. Recent findings indicate that nitric oxide can modulate angiogenesis, immune responses, and extracellular matrix remodeling within tumors, all of which are vital for tumor development and therapeutic response. By understanding how nitric oxide interacts with various components of the tumor microenvironment, researchers can identify potential therapeutic targets for intervention and treatment.
For instance, nitric oxide’s influence on angiogenesis can significantly impact tumor growth and metastasis, making it a valuable target for therapeutic strategies aimed at disrupting the blood supply to tumors. Additionally, nitric oxide’s role in modulating immune responses within the tumor microenvironment underscores its potential as a means of enhancing anti-tumor immunity. As research progresses, the opportunity to develop nitric oxide-based therapies that target the tumor microenvironment offers exciting possibilities for improving cancer treatment and patient outcomes, thereby revolutionizing cancer care.
Frequently Asked Questions About Nitric Oxide and Its Applications
What is nitric oxide, and why is it vital for health?
Nitric oxide is a signaling molecule produced in the body that plays a crucial role in various physiological processes, including vasodilation, neurotransmission, and immune responses. Its significance lies in its ability to regulate blood flow, enhance oxygen delivery, and modulate inflammation, making it essential for maintaining overall health and well-being.
How does nitric oxide influence cardiovascular health?
Nitric oxide promotes vasodilation, which improves blood flow and reduces blood pressure. It also supports endothelial function, inhibits platelet aggregation, and contributes to overall cardiovascular health, making it crucial for preventing heart disease and other vascular conditions that can threaten well-being.
What neuroprotective effects does nitric oxide provide?
Nitric oxide has been shown to protect neurons from damage by modulating various cellular processes. It can mitigate oxidative stress, enhance neuronal survival, and promote repair mechanisms in response to injury, making it a key player in neurological health and the prevention of neurodegenerative diseases.
How does nitric oxide contribute to respiratory health?
Nitric oxide aids in lung function by promoting vasodilation and improving blood flow in the lungs. It also possesses bronchodilatory effects that help alleviate symptoms in conditions like asthma and pulmonary hypertension, enhancing overall respiratory performance and patient comfort.
Can nitric oxide be employed as an antimicrobial agent?
Yes, nitric oxide has demonstrated antimicrobial properties that enable it to combat various pathogens, including bacteria and viruses. Its ability to disrupt microbial membranes and modulate immune responses positions it as a valuable tool in infection control strategies, addressing the rising challenge of antibiotic resistance.
What potential does nitric oxide hold in cancer research?
Nitric oxide exhibits a dual role in cancer biology, influencing both tumor growth and suppression. It may serve as a therapeutic agent by inducing cancer cell death while also affecting the tumor microenvironment and angiogenesis, presenting opportunities for targeted cancer therapies that improve treatment effectiveness.
Are there clinical applications for nitric oxide therapy?
Yes, nitric oxide therapy is being explored for various clinical applications, including treating pulmonary hypertension, enhancing wound healing, and developing targeted cancer therapies. Ongoing clinical trials are evaluating its safety and efficacy across these contexts, aiming to translate research findings into practical health solutions.
What are the latest advancements in nitric oxide research?
Recent advancements encompass the discovery of new enzymatic pathways for nitric oxide synthesis, improved production techniques, and the development of novel catalysts. These breakthroughs enhance our understanding and application of nitric oxide in medicine and health, paving the way for innovative therapies.
How does nitric oxide influence neuroinflammation?
Nitric oxide plays a dual role in neuroinflammation, promoting both protective and inflammatory responses. Its regulation is crucial for maintaining neuronal health and preventing the onset of neurodegenerative diseases, emphasizing the need for balanced signaling and therapeutic interventions.
What future directions are anticipated for nitric oxide research?
Future research directions include exploring nitric oxide’s applications in infection control, cancer therapy, and enhancing delivery methods for increased efficacy. Studies are also focused on understanding its complex interactions within biological systems to develop targeted therapies that improve patient care and health outcomes.
Connect with us on Facebook!
The Article Nitric Oxide Research Updates: Latest Discoveries appeared first on https://athleticsupplement.com
The Article Nitric Oxide Research: New Discoveries and Insights Was Found On https://limitsofstrategy.com